The slit lamp biomicroscope is the most frequently used diagnostic tool for veterinary ophthalmologists. It provides magnified, three-dimensional examination of the ocular adnexa, cornea, anterior chamber, lens, and vitreous humor. Its purpose is to allow continuous examination under magnification, using various illumination methods to identify conditions as thoroughly as possible and understand the entire ocular structure, including the fundus and adnexa.
Currently, common slit lamp examination methods can be categorized into six types. The difference in examination methods primarily depends on the direction, scope, intensity, and position of the slit lamp's light source and background light source, as well as the shape of the light source. Therefore, they are often named according to the characteristics of their illumination.
1. Diffuse Illumination
Diffuse illumination is the most basic lighting method. It's particularly well-suited for low to medium magnification examinations of large abnormal areas, and for the initial assessment of the cornea, anterior chamber, and iris. If you find conditions like foreign bodies, ulcers, pigmentation, or edema, you can note them and then proceed with more targeted methods and higher magnification for detailed examination.
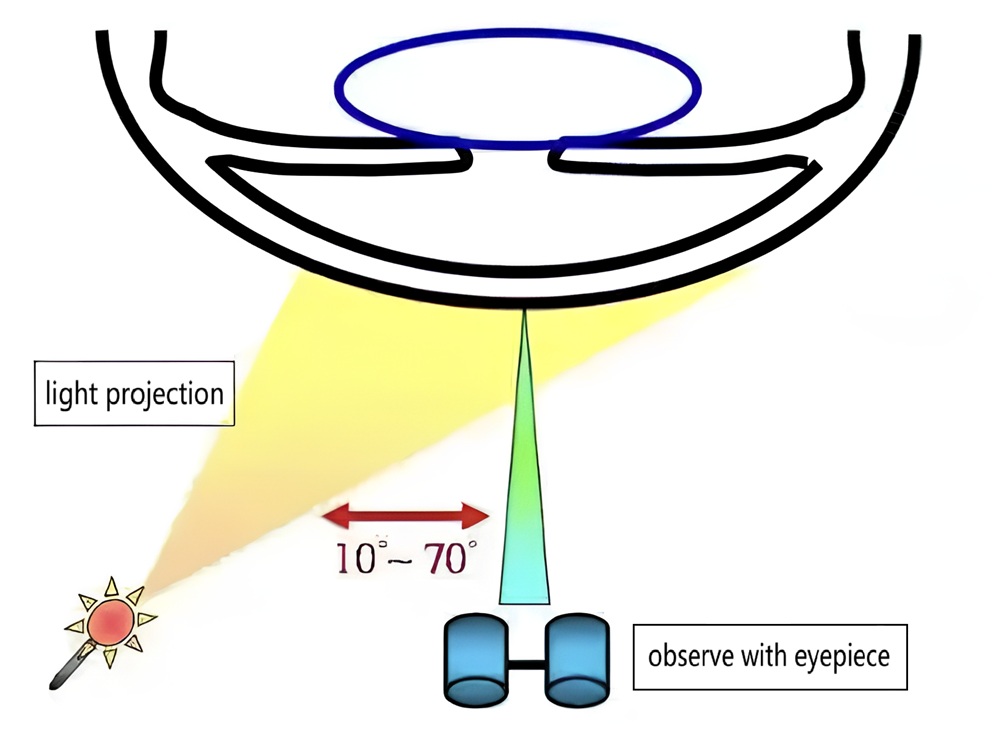
▲ Schematic Diagram of Diffuse Illumination
- Slit Width: **
- Slit Angle: 10°–70°
- Magnification: Low, with further magnification for detailed observation
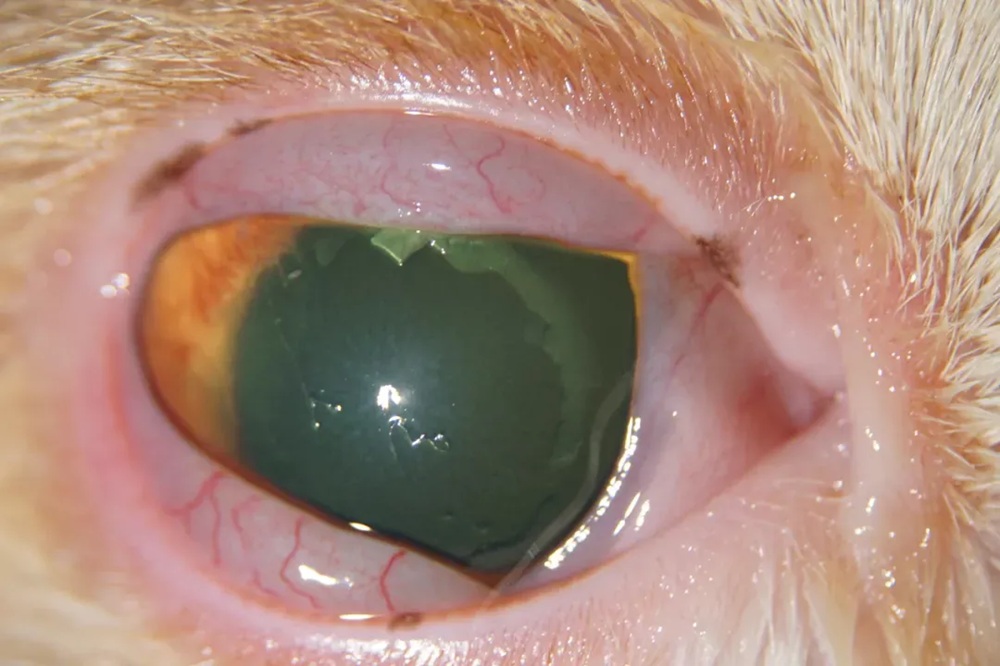
▲ Diffuse illumination observing conjunctival swelling in a cat, extensive corneal epithelial erosion, and neovascularization

▲ Diffuse illumination in a dog case of canine uveitis, showing conjunctival hyperemia and mild anterior chamber turbidity.
2. Direct Focal Illumination
Direct focal illumination is the foundational and most frequently used method for slit lamp biomicroscopy. All other methods are derived from it. This technique involves superimposing the light source's illuminated area with the microscope's focal point, then adjusting the slit width for observation.
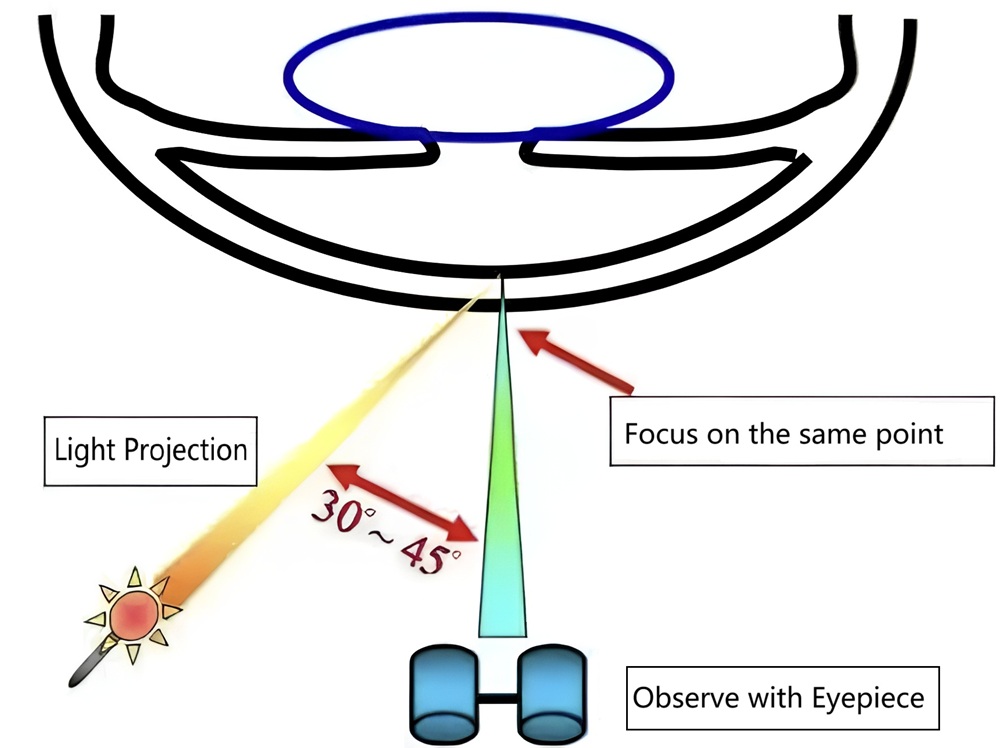
▲ Schematic Diagram of Direct Focal Illumination
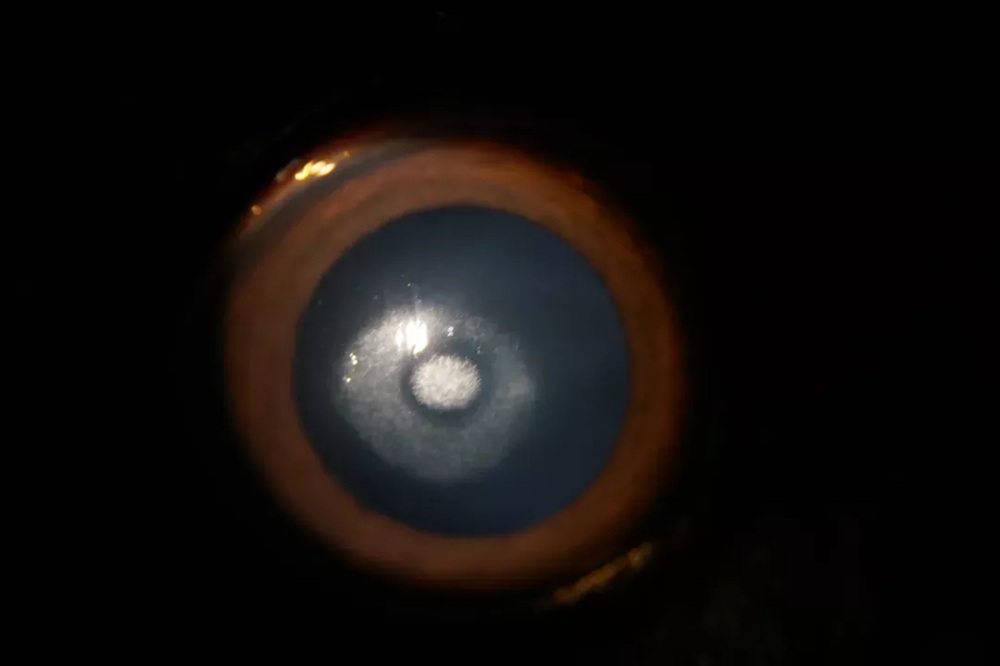
▲ Direct focal illumination revealing central corneal white crystalline opacity
- Slit Width: 1–2 mm, >5 mm
- Slit Angle: 30°–45°
- Magnification: 10x or higher
Choosing Between Wide and Narrow Slit Beams
-Application: When examining with a wide slit beam, transparent ocular structures become visible. Wide beam illumination is suitable for preliminary assessment of the overall corneal status, observing opacities within the cornea, and conducting general eye examinations.
- Advantages: By providing a broader field of view, wide beam illumination helps in observing the overall condition of ocular structures like the cornea. When examining deeper structures, a wide beam is better at detecting structural abnormalities.

▲ Wide beam illumination for assessing corneal edema
- Application: A narrow slit beam creates an optical section that provides detailed information about the cornea's epithelium, stroma, and endothelium. Narrow beam illumination is especially suitable for a fine, detailed examination of transparent ocular tissues like the cornea, anterior chamber, and lens.
- Advantages: By producing a thin optical section, narrow beam illumination allows the clinician to observe specific details of ocular structures, such as different corneal layers and deeper structures, which helps in identifying and assessing subtle lesions.
▲ Narrow beam illumination detecting anterior chamber flare

▲ Narrow beam illumination highlighting a deep corneal ulcer
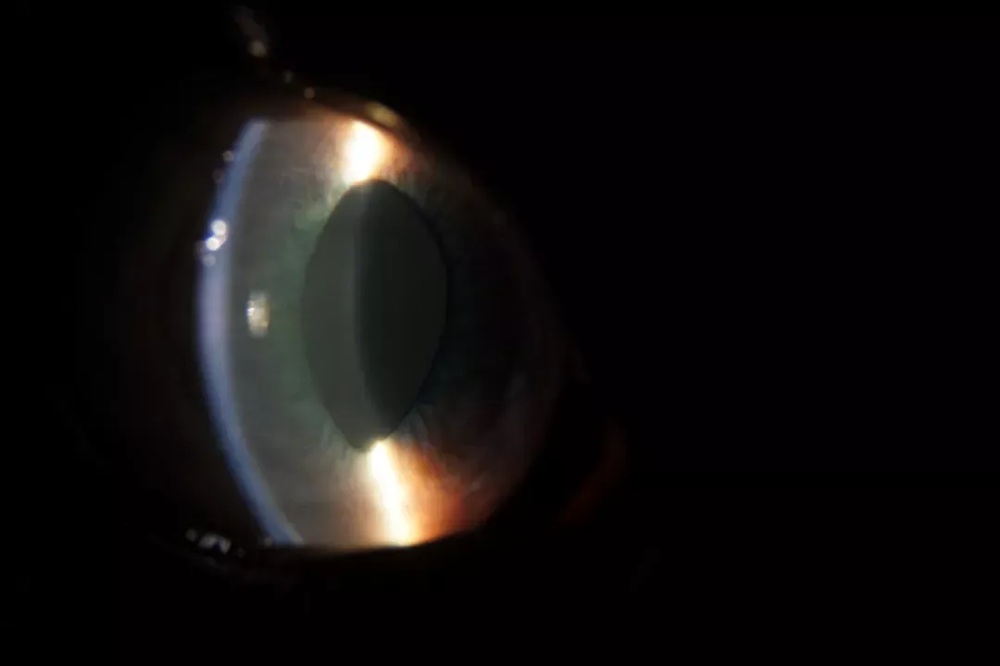
3. Retro-Illumination
Retro-illumination involves directing the slit lamp's light source behind the tissue being examined. It's a commonly used method for inspecting ocular tissues and structures by observing light reflected or scattered from the posterior structures. This technique is often employed to visualize subtle lesions . For example, by directing the light source onto the iris or lens, reflected light can be used to observe corneal lesions, such as corneal neovascularization. When animals develop cataracts, retro-illumination clearly reveals the opaque areas of the lens.
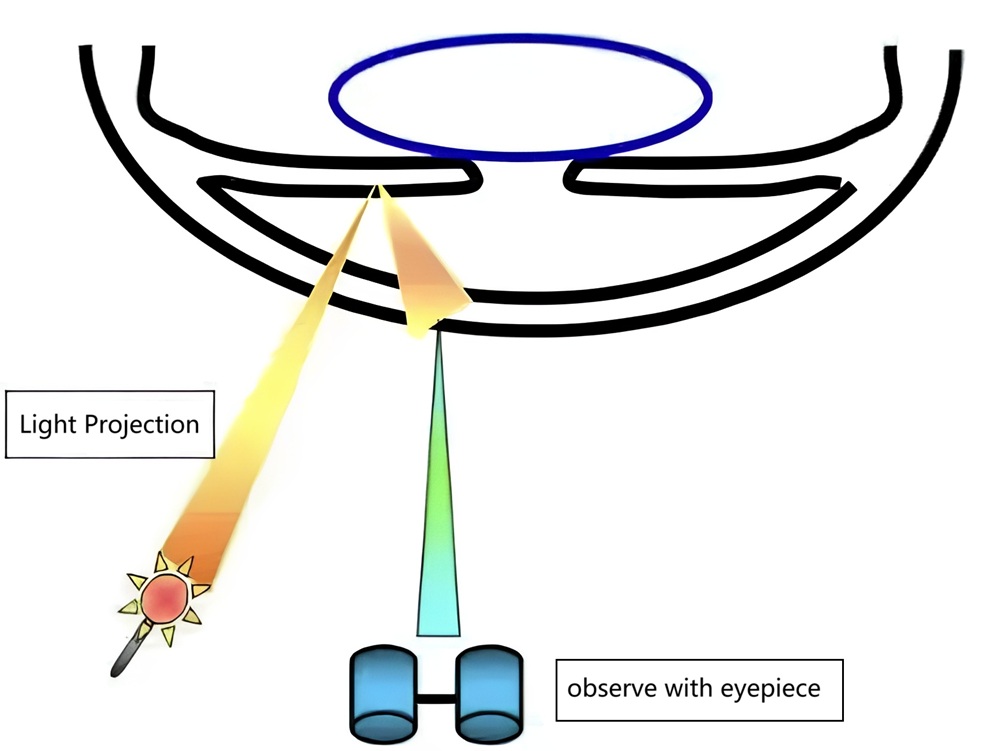
▲ Schematic diagram of Retro-Illumination
▲ Retro-illumination demonstrating an immature cataract and lens subluxation
- Slit Width: 3–4 mm
- Slit Angle: 15° (adjustable)
- Magnification: 10x or higher
4. Indirect Illumination
Indirect illumination involves directing the slit lamp's light source near the tissue being examined, illuminating it through light scattering and reflection. A large angle between the incident light and the observation line, combined with slow movement of the light, will aid in observation. This method is often used to observe lesions such as intra-iridal hemorrhage, iris vessels, corneal bullae, and blood vessels.
▲ Schematic diagram of Indirect Illumination
▲ Indirect illumination visualizing a corneal ulcer
- Slit Width: 3–4 mm
- Slit Angle: 30°–45°
- Magnification: 10x or higher
5. Specular Reflection Illumination
Specular reflection illumination fully utilizes the specular reflection zone produced by the slit lamp's light source on the corneal or lenticular surface. This zone is superimposed with the optical parallelepiped from direct focal illumination. By leveraging the increased luminosity in this area, the tissue can be examined. This method is commonly used to observe corneal endothelial cells and typically requires a table-top slit lamp for observation.
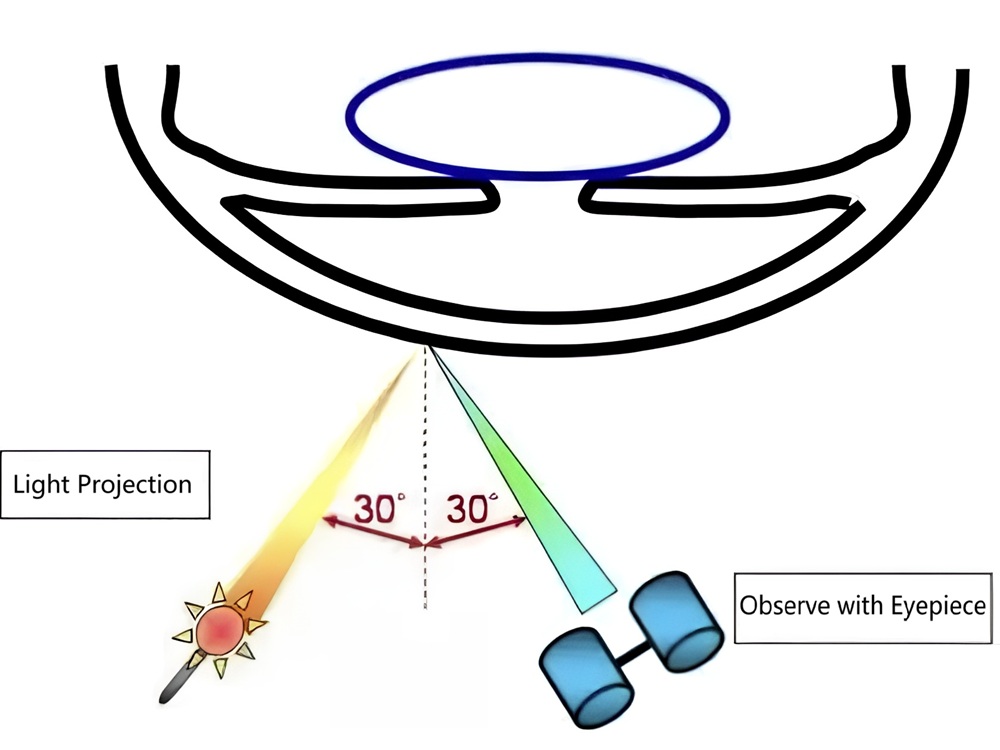
▲ Schematic diagram of Specular Reflection Illumination
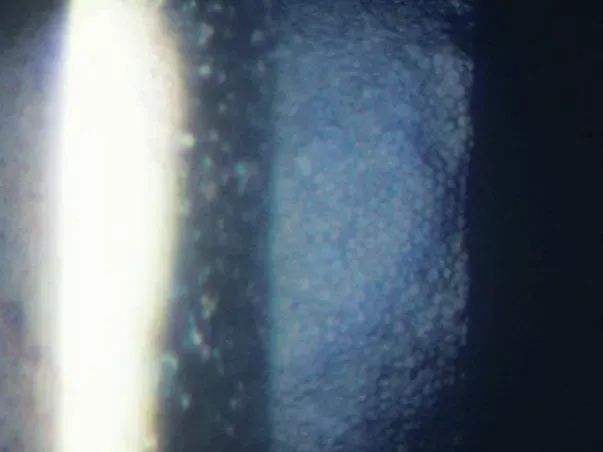
▲ Specular reflection illumination examining the human corneal endothelium
- Slit Width: 1 mm
- Slit Angle: ~60° (fine-tuned)
- Magnification: Low magnification for initial focus, gradually increased to 40x
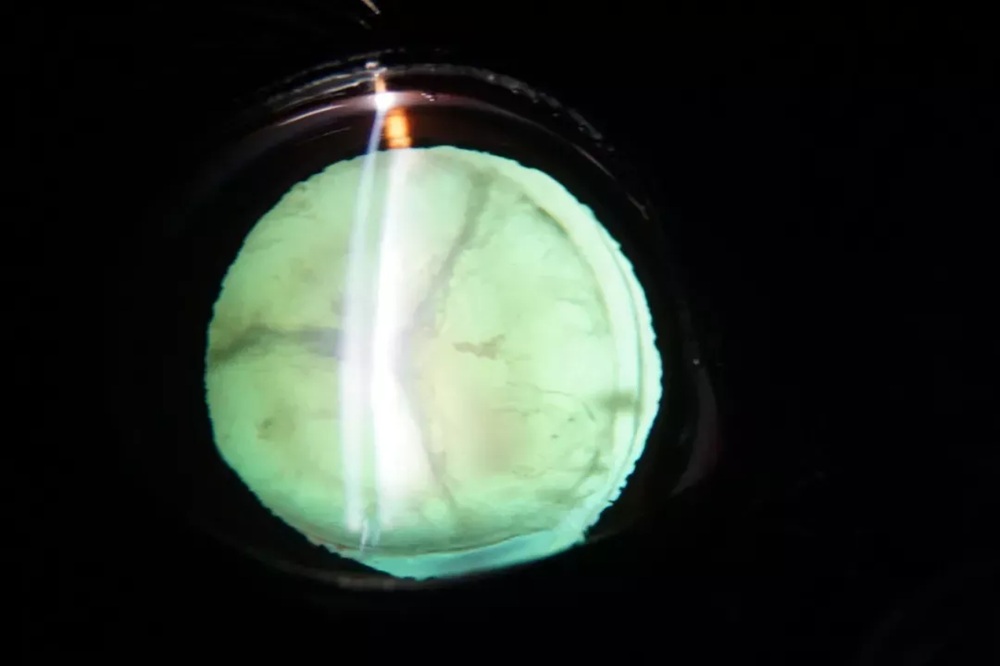
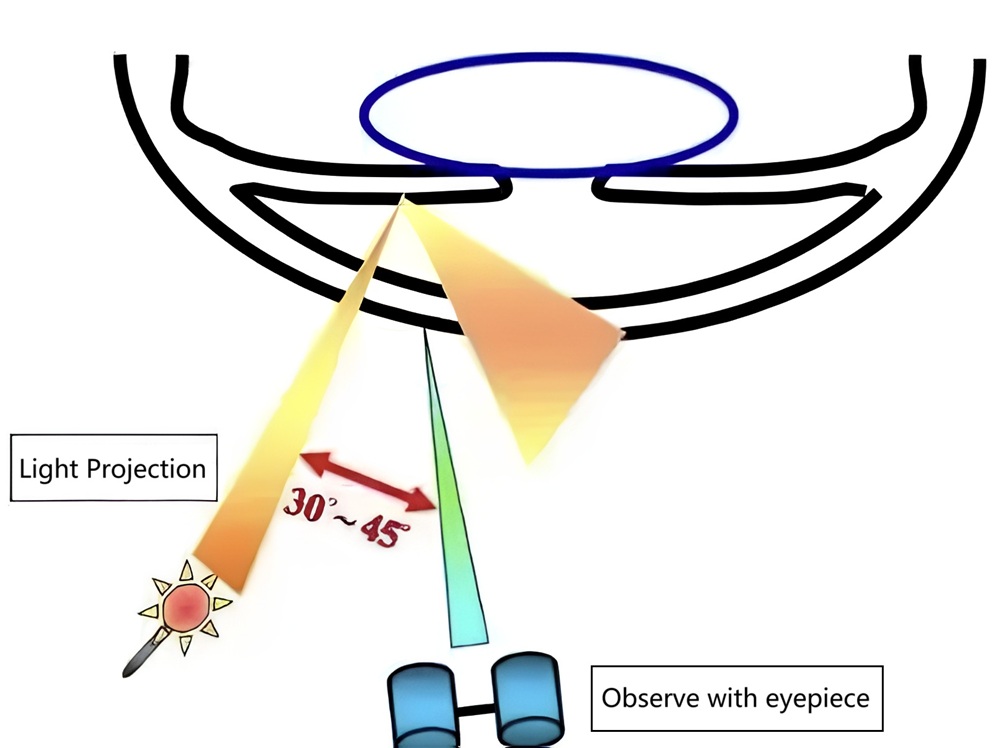
6. Corneoscleral Scatter Illumination
Corneoscleral scatter illumination utilizes the principle of total internal reflection of light and the transparent nature of the cornea. The slit lamp light source is directly projected onto the limbus (corneoscleral junction). The light then undergoes total internal reflection within the corneal tissue, forming a halo around the limbus. By focusing the microscope on the cornea, the transparency of the corneal tissue can be clearly visualized, with the opposite limbus appearing brightest. This method is suitable for examining subtle changes in the cornea and is commonly used to check for corneal precipitates, corneal infiltrates, and corneal bullae.
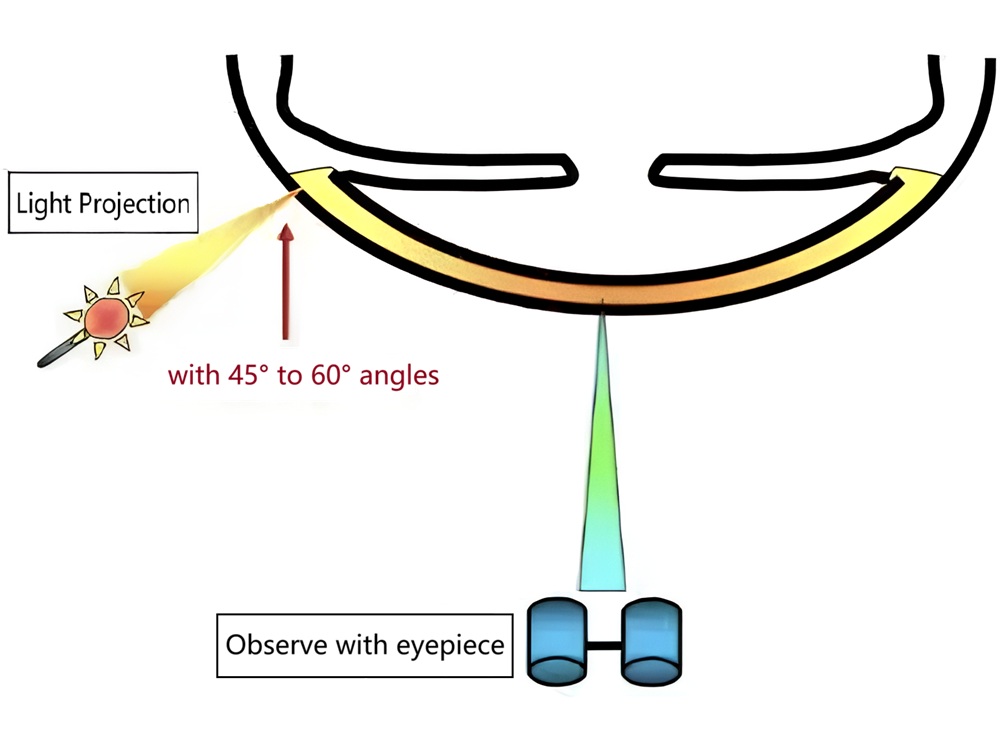
▲ Schematic diagram of Corneoscleral Scatter Illumination
- Slit Width: 3–5 mm
- Slit Angle: 45°–60°
- Magnification: 10x or higher
References
Note: Slit width and angle can vary based on equipment specifications and clinical requirements. Adjustments must be tailored to each case.

