What is Intraocular Pressure (IOP)?
Intraocular pressure (IOP) is the pressure exerted by the contents of the eye (including the lens, vitreous body, uvea, retina, and the intraocular fluids—aqueous humor and blood) against the inner wall of the eyeball. It is measured in millimeters of mercury (mmHg). Among these components, the aqueous humor circulation has the most significant impact on IOP.
How Is IOP Obtained?
Measuring IOP is one of the most crucial examinations in ophthalmology.
IOP measurement isn’t solely for diagnosing glaucoma (elevated IOP) in affected animals; it can also be used to diagnose uveitis (decreased IOP).
Furthermore, it helps differentiate causes of red eye, such as keratitis, conjunctivitis, or scleritis, which typically do not affect IOP.
In clinical practice, tonometers are commonly used to measure IOP. The tonometers frequently used in veterinary clinics include the applanation tonometer and the rebound tonometer.
If you’d like to learn more about our tonometer products, please feel free to contact us. We can provide recommendations based on your specific needs.
What is Normal IOP?
Normal IOP, also known as intraocular pressure, is the pressure exerted by the contents of the eye (including the lens, vitreous body, uvea, retina, and intraocular fluids—aqueous humor and blood) against the inner wall of the eyeball.
It is expressed in millimeters of mercury (mmHg), with aqueous humor circulation having the most significant impact on this pressure.
“Normal IOP” is a statistical concept derived from sampling surveys of healthy populations, rather than a simple numerical category. It is a physiological indicator that exhibits both inter-individual and intra-individual variation.
The reference range for normal animal IOP is typically established by measuring and statistically analyzing IOP data from a select number of healthy animals.
From a clinical perspective, the definition of normal IOP should be “the range of intraocular pressure that does not cause glaucomatous optic nerve damage.”
Pathologically elevated IOP is only defined as such when the pressure exceeds the individual optic nerve’s tolerable limit, leading to optic nerve damage and visual field impairment.
IOP Reference Range
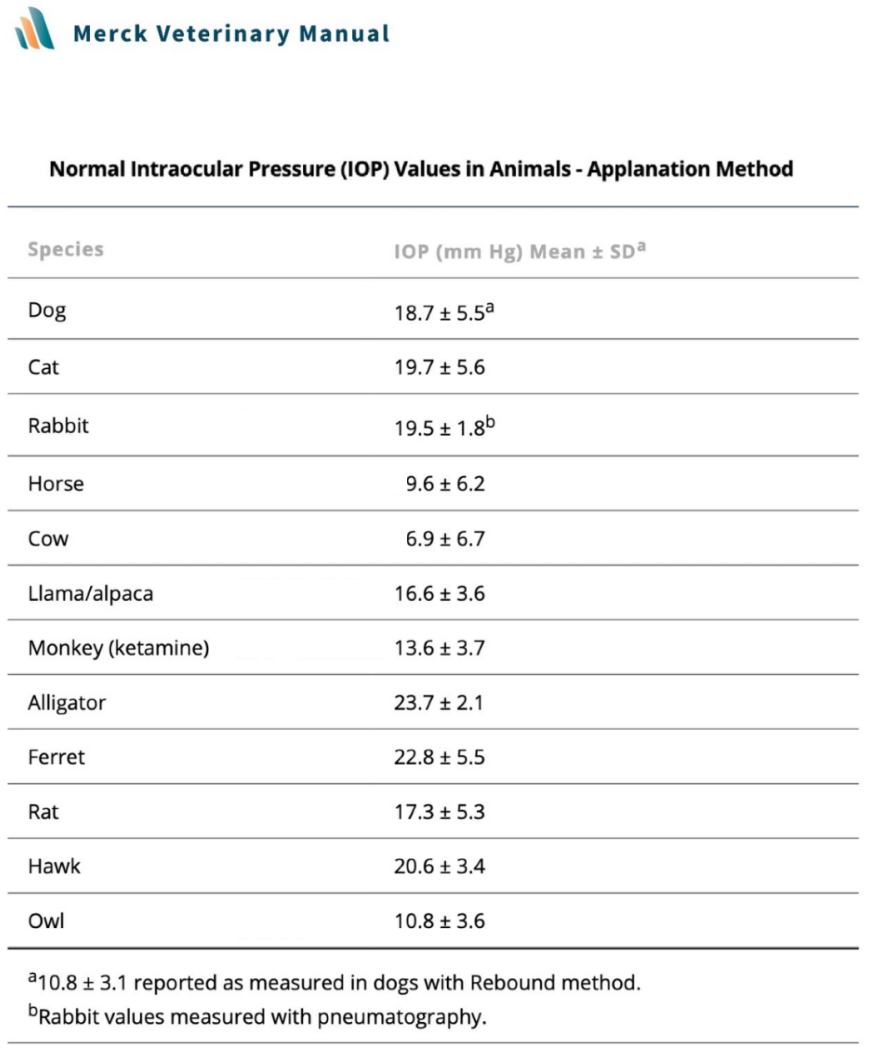
Normal intraocular pressure-Merck Veterinary Manual
For animal eyes, there isn’t an absolute distinguishing value between a healthy eye and a diseased eye. The “normal” IOP range serves only as a reference guideline and requires comprehensive evaluation in conjunction with other ophthalmic examinations. IOP should always be measured in both eyes.
Clinical Significance
In clinical practice, the interpretation of animal IOP results should not overly rely on the “normal” IOP range.
1. Physiological Variations (↑↓)
- Circadian Rhythm: In dogs, normal IOP is highest in the morning and gradually decreases throughout the day. For cats and rabbits, normal IOP is lowest in the afternoon and highest at night. In horses, normal IOP is higher during the day and lower at night (influenced by light-dark cycles).
- Age: An animal’s normal IOP value tends to decrease with age.
- Reproductive Status: In female cats, IOP significantly increases during estrus (heat).
2. Pathological Increases (↑)
- Glaucoma: Glaucoma is a disease where elevated intraocular pressure leads to optic nerve damage, commonly seen in dogs, cats, and other animals.
- Anterior Uveitis: Anterior uveitis is inflammation of the front part of the eye, which can cause increased IOP. It’s very common in dogs, cats, and other animals.
- Tumors: Ocular or periocular tumors can compress eye structures, leading to elevated IOP, commonly observed in dogs, cats, and other animals.
- Lens Luxation: Lens luxation refers to the displacement of the lens, often into the anterior chamber, which can cause increased IOP. This is frequently seen in dogs, cats, and other animals.
- Hyperthyroidism: Hyperthyroidism can cause exophthalmos (protrusion of the eyeball) and compression, leading to elevated IOP. This is relatively common in dogs, cats, and other animals.
- Hyphema (Intraocular Hemorrhage): Blood in the anterior chamber (hyphema) can lead to secondary glaucoma and elevated IOP. This is relatively common in dogs, cats, and other animals.
- Other Diseases: Conditions such as connective tissue diseases, liver disease, and kidney disease can also lead to increased IOP, commonly found in dogs, cats, and other animals.
It’s important to note that the pathological factors listed above may not be the sole causes of elevated IOP, and other factors can also affect normal IOP levels. Therefore, clinical diagnosis and treatment require a comprehensive assessment and management based on the specific situation.
3. Pathological Decrease (↓)
- Post-Surgical or Traumatic Wound Leakage, Ciliary Body Detachment, Ocular Perforation, Severe Iridocyclitis, Retinal or Choroidal Detachment: These conditions can lead to a decrease in IOP.
- Excessive Aqueous Humor Filtration after Glaucoma Filtering Surgery: This can result in IOP being too low.
- Systemic Conditions: Conditions such as myotonic dystrophy and those causing hyperosmolarity of the blood, including dehydration, uremia, and diabetes, can also lead to decreased IOP.
- Vascular Occlusive Diseases: Conditions like ocular ischemic syndrome, giant cell arteritis, and central retinal vein or artery occlusion can cause a drop in IOP.
- Uveitis Leading to Ciliary Body Shutdown (Shock): Generally, IOP tends to decrease with uveitis. However, in cases of severe uveitis, IOP might remain within the normal range or even show a tendency to increase. When this occurs, the possibility of secondary glaucoma must be considered, and appropriate management should be implemented.
Influencing Factors
- Animal Restraint: Pulling on the eyelids or applying pressure to both jugular veins can significantly increase IOP values. This is because jugular vein compression leads to increased pressure in the episcleral venous system, resulting in venous stasis.
- Medication Effects: Veterinarians should be aware of how various medications can affect animal IOP. For example, topical tropicamide can significantly raise IOP in both healthy and glaucomatous cats. Compared to cats, topical tropicamide has less impact on IOP in dogs.
- Measurement Order: The IOP measured in the first eye (whether right or left) is consistently higher than that of the contralateral eye. Repeated IOP measurements during the same visit may lead to a noticeable decrease in IOP, although the magnitude might not always be clinically significant.
Disclaimer:
This article is for the purpose of learning and exchanging knowledge in animal ophthalmology only, and does not constitute diagnostic or treatment advice.
References:
[1] Wang Shuangning, Zhou Weiwei. Research Progress on the Influence of Cardiovascular Disease Risk Factors on Intraocular Pressure [J]. Guangxi Medical Journal, 2022, 44(21): 2564-2566+2584.
[2] Dong Yi, Lin Zhongtian. Small Animal Ophthalmology [M]. Beijing: China Agricultural Press, 2013: 18.
[3] Ren Zeqin. The Understanding of “Normal Intraocular Pressure” Needs to Be Deepened [J]. Ophthalmology, 2008(01): 6-9.
[4] https://wsjk.ln.gov.cn/wsjk/index/syxwxx/mtbb/2023030815465158831/index.shtml
[5] Giannetto, C., Piccione, G. and Giudice, E. (2009), Daytime profile of the intraocular pressure and tear production in normal dog. Veterinary Ophthalmology, 12: 302-305. https://doi.org/10.1111/j.1463-5224.2009.00717.x
[6] Del Sole, M.J., Sande, P.H., Bernades, J.M., Aba, M.A. and Rosenstein, R.E. (2007), Circadian rhythm of intraocular pressure in cats. Veterinary Ophthalmology, 10: 155-161. https://doi.org/10.1111/j.1463-5224.2007.00525.x
[7] https://doi.org/10.1016/0014-4835(77)90149-X.
[8] Bertolucci, C., Giudice, E., Fazio, F., & Piccione, G. (2009). Circadian intraocular pressure rhythms in athletic horses under different lighting regime. Chronobiology international, 26(2), 348–358. https://doi.org/10.1080/07420520902751035
[9] Kato, K. (2014), Comparison of two handheld applanation tonometers and the association of central corneal thickness, age, and intraocular pressure in normal and diseased canine eyes. Vet Ophthalmol, 17: 417-425. https://doi.org/10.1111/vop.12151
[10] Ofri, R., Shub, N., Galin, Z., Shemesh, M., & Shore, L. S. (2002). Effect of reproductive status on intraocular pressure in cats. American journal of veterinary research, 63(2), 159–162. https://doi.org/10.2460/ajvr.2002.63.159
[11] (Japan) Yudo Takuya. Companion Animal Ophthalmology [M]. Translated by Chen Wu, Fu Yuan, Xia Nan. Wuhan: Hubei Science and Technology Press, 2018: 206.
[12] Klein, H. E., Krohne, S. G., Moore, G. E., Mohamed, A. S., and Stiles, J. (2011). Effect of eyelid manipulation and manual jugular compression on intraocular pressure measurement in dogs. Journal of the American Veterinary Medical Association 238, 10, 1292-1295, available from: < https://doi.org/10.2460/javma.238.10.1292>
[13] Bigger JF. Glaucoma with elevated episcleral venous pressure. Southern Medical Journal. 1975 Nov;68(11):1444-1448. DOI: 10.1097/00007611-197511000-00026. PMID: 1188433.
[14] Feline Ophthalmology / (UK) Natasha Mitchell, (UK) James Oliver (Editors); Chief Translators Zhou Xiaofei, Song Xiaojing. Shenyang: Liaoning Science and Technology Press, 2023: 130.
[15] Oren Pe’er, Eni Chiu, Dikla Arad, Cristina Lelescu, Maya Ross, Ron Ofri, Does the order of intraocular pressure measurement affect tonometry results?, Veterinary Ophthalmology, 10.1111/vop.12861, 24, S1, (146-153), (2021).
