Introduction
Intraocular pressure (IOP) measurement is a cornerstone of veterinary ophthalmic diagnostics. However, numerous physiological, anatomical, environmental, and technical factors can significantly influence the accuracy and interpretation of IOP values. Understanding these variables is crucial for practitioners to avoid misdiagnosis and to monitor ocular diseases effectively.
Instrument-Related Factors
Type of Tonometer and Its Principles
IOP readings can vary depending on the tonometer used. As described in Veterinary Ophthalmology, “The ideal tonometer should be easy to use, atraumatic, require minimal restraint, and provide accurate and repeatable estimates of IOP in both normal and diseased eyes. Tonometers designed for use in veterinary medicine should also be accurate across a wide range of species with different ocular anatomy.
Differences in measurement technique—indentation, applanation, and rebound tonometry—result in variability due to assumptions regarding corneal thickness, curvature, rigidity, and even tear film viscosity and temperature. For instance, the Tono-Pen (applanation) is “very accurate in the physiologic range, but tends to overestimate IOP in the low range and underestimate IOP in the high range in dogs, cats, and humans,” while the TonoVet (rebound) “underestimated the IOP by 37%–60% in enucleated rabbit eyes and 17%–63% in enucleated porcine eyes, as compared to direct manometry.
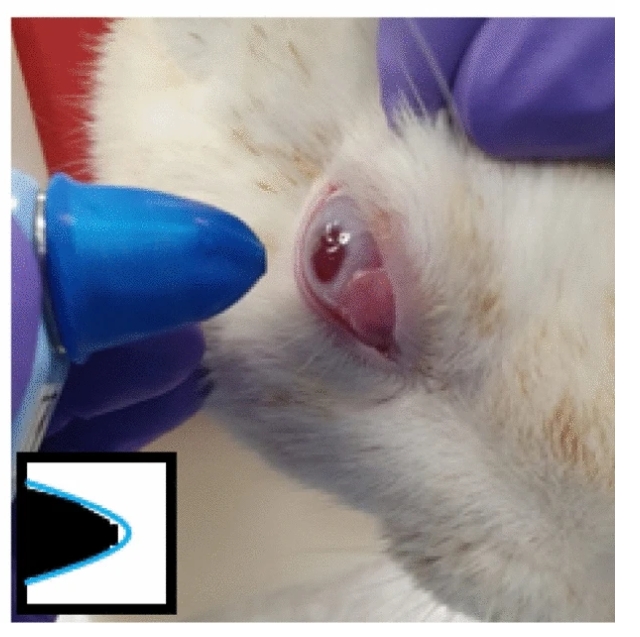
Intraocular Pressure Measurement
Calibration and Device Maintenance
Accurate calibration is essential, as “failure to follow manufacturer instructions for maintenance and calibration may result in systematically inaccurate readings.” Always verify that the instrument is clean, properly zeroed, and fitted with a new tip or probe for each patient.
Patient-Related Factors
Species, Breed, and Individual Variability
Species and breed differences influence IOP readings due to anatomic diversity in corneal thickness, curvature, and scleral rigidity. For example, “the normal range of IOP in most animals is somewhere between 15 and 25 mmHg because of the conservation between species,” yet values can differ: dog (15–18 mmHg), cat (17–19 mmHg), rabbit (15–20 mmHg), horse (17–28 mmHg).
Scleral elasticity is greater in dogs and cats compared to adult humans, causing less resistance to indentation tonometry. Ocular rigidity may also be altered by age, disease, or previous surgery, thus affecting IOP measurements.
Age, Gender, and Physiological State
Age can influence IOP: “there is a negative association between age and IOP (in contrast to a positive association between age and tear production). This is true for the dog, cat, and camel, but not for the lion and sambar deer In dogs, IOP declines by 2–4 mmHg as age increases from less than 2 years to greater than 6 years. IOP is considerably lower in geriatric cats than in young cats, and higher in adolescent cats than in adults.
Most studies show no gender effect, but some exceptions exist (e.g., higher IOP in male lions and in cats/lions in certain reproductive phases).
Circadian Rhythm and Diurnal Variations
Circadian and diurnal rhythms produce measurable IOP fluctuations. In dogs, IOP peaks in the morning; in cats, maximal values are detected at night, gradually declining through the day. Horses show low IOP during dark phases and high during the light, with a peak at the end of the light phase.
Environmental and Handling Factors
Restraint, Sedation, and Anesthesia
Physical or chemical restraint, as well as patient positioning, can significantly alter IOP. “The method of restraint (physical or chemical) and body and head position can also have a dramatic effect Excessive restraint or pressure—especially on the neck or jugular veins—may falsely elevate IOP, particularly in brachycephalic dogs. “IOP in dogs is significantly increased by applying neck pressure via a collar but not via a harness.” Eyelid manipulation and manual compression of the jugular vein(s) can also cause large IOP increases.
In horses, IOP decreases with xylazine sedation, while ketamine increases IOP in dogs; the effects of other sedatives or anesthetics can be variable and sometimes substantial.
Body and Head Position
Body position alters IOP values.
- In dogs, sternal recumbency maintains stable IOP, while dorsal recumbency or sitting positions are associated with decreasing IOP during examination.
- In horses, IOP is significantly higher when the head is below heart level.
- In small mammals, upright position is often best for reliable readings.
Ocular Surface and Pathology
Corneal Thickness and Pathology
Corneal thickness (central corneal thickness, CCT) can significantly affect IOP results, especially with applanation and rebound tonometry. “For every 100 μm increase in corneal thickness, the IOP increases by 1 mmHg for the Tono-Pen XL and 2 mmHg for the TonoVet.” However, results vary among devices and studies; some report minimal influence when using default calibration settings.
Corneal pathology—such as edema, ulceration, or scarring—may produce unreliable readings. “If corneal pathology is present, it is prudent to take readings from the most normal part of the cornea. This factor is affected by the size of the footplate of the tonometer: the small area of the rebound tonometer probe and Tono-Pen tip are more advantageous than the large footplate of the Schiøtz tonometer.
Topical Medications
- Topical drugs, particularly mydriatics like tropicamide and atropine, can substantially raise IOP in cats and, to a lesser extent, in dogs.
- Topical tropicamide 1% has been shown to cause a substantial increase in IOP (up to 6–7 mmHg) in both normal and glaucomatous cats.
- In dogs, the effect is less, but clinically relevant increases can still occur Cyclopentolate, on the other hand, does not significantly alter IOP and can be considered safer if cycloplegia is needed.
Technical and Operator Factors
Experience and Technique
Operator skill plays a critical role. Inexperienced users are more likely to obtain inaccurate or inconsistent IOP readings. For example, “a study using a cadaveric cornea eye model showed that an experienced examiner could estimate IOP within 5 mmHg 100% of the time, as compared with 62% for an inexperienced examiner Proper training and adherence to technique—avoiding digital pressure, ensuring correct alignment, and performing serial measurements—are essential.
Device Positioning and Repeatability
Accurate tonometry requires the device probe to be perpendicular to the central cornea, with minimal pressure applied elsewhere on the eye or lids. Misalignment or repeated measurement at the same site can cause artifact. Regularly compare both eyes, as a difference of more than 8 mmHg is usually abnormal.
Biological and Environmental Variables
Circadian and Seasonal Effects
IOP fluctuates not only throughout the day but may vary with season. Although less dramatic than circadian effects, such variations have been described and should be considered when monitoring chronic ocular disease.
Other Physiological Factors
Reproductive status and body length have been shown to affect IOP in some exotic species (e.g., higher IOP in alligators ≤50 cm in length). Disease states, systemic health, and hydration may also contribute to variation.

