Porcine Small Intestinal Submucosa (SIS) for Deep Melting Corneal Ulcers in Dogs and Cats: Clinical Outcomes and Healing Characteristics
Deep melting corneal ulcers are one of the most severe ophthalmic emergencies in dogs and cats. Characterized by rapid stromal liquefaction driven by bacterial proteases (especially Pseudomonas aeruginosa), fungal elements, or excessive host matrix metalloproteinases (MMPs), these ulcers can progress to descemetocele or perforation within hours to days. When medical therapy alone fails to halt progression, surgical reconstruction becomes mandatory.
Case Series Overview
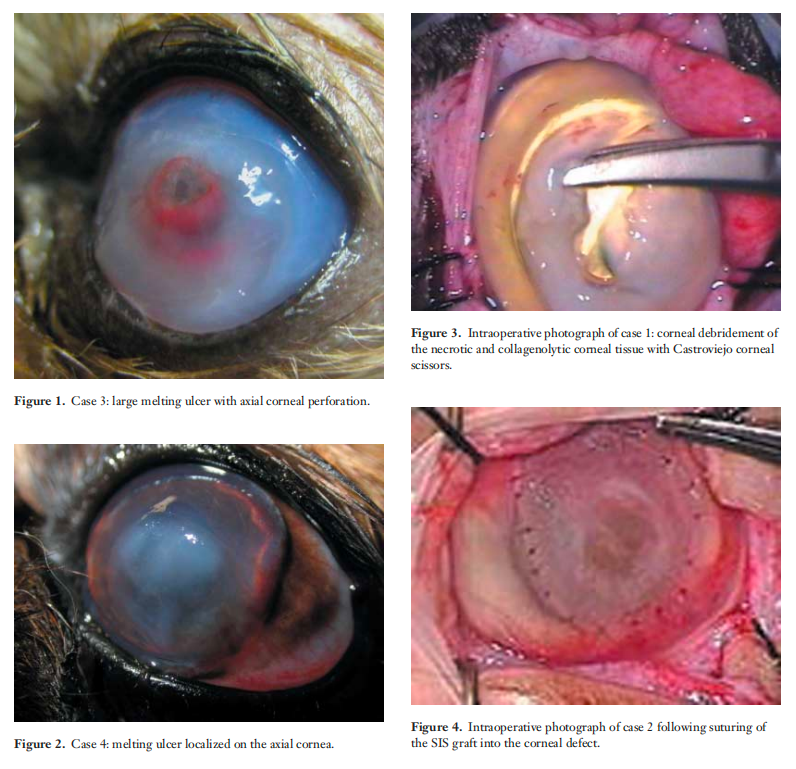
Seven animals (5 dogs, 2 cats; 2–9 years old) with rapidly progressing deep melting ulcers were treated using multilayer porcine small intestinal submucosa (SIS) grafts. Two eyes (1 cat, 1 Shih Tzu) already presented with corneal perforation at referral. Most canine cases were trauma-related; one dog had concurrent keratoconjunctivitis sicca (KCS). One cat was FHV-1 PCR-positive with dendritic lesions in the fellow eye.
Surgical Technique – Porcine SIS Grafting
Under operating microscopy, all necrotic and liquefied stroma was meticulously debrided. Rehydrated porcine SIS sheets were trimmed 1 mm larger than the defect and secured to healthy corneal margins with 9-0 Vicryl simple interrupted sutures (cardinal sutures first at 12-3-6-9 o’clock). A third-eyelid flap was placed in six of seven cases for protection.
Key Pathophysiologic Drivers of Melting
- Overwhelming MMP and neutrophil elastase activity
- Bacterial exotoxins (Pseudomonas aeruginosa most common)
- Trauma or viral epithelial compromise (FHV-1)
- Tear film deficiency or qualitative tear abnormalities
Postoperative Healing Timeline
Day 15
- Fluorescein-negative in 100 % of cases (complete epithelialization)
- Neovascularization present in all eyes
- Graft well positioned; one minor partial dehiscence without loss of globe curvature
Week 4
- Graft shows characteristic opaque-milky appearance
- Intense stromal cellular proliferation and remodeling
Days 35–45
- Progressive graft integration
- Superficial vessels begin to regress
Months 2–3
- Smaller defects regain near-complete transparency
- Larger/perforated defects show mature granulation that continues to clear
- Two perforated cases developed anterior synechiae but retained functional vision
Month 6 – Final Outcome
- 5/7 eyes achieved fully transparent corneas
- 7/7 eyes regained sufficient transparency for normal visual function
- 100 % vision preservation, including both perforated cases
Biological Advantages of Porcine SIS in Corneal Reconstruction
- Provides immediate tectonic support even in perforated globes
- Rich in collagen I/III/V, fibronectin, hyaluronic acid, and growth factors (TGF-β1–3, bFGF)
- Promotes rapid keratocyte repopulation and orderly ECM remodeling
- Low antigenicity → minimal inflammatory response
- Final transparency far superior to conjunctival grafts
Reported Complications (Rare in This Series)
- Graft dehiscence, persistent uveitis, endophthalmitis, or third-eyelid flap failure have been described in larger series but did not occur here.
Conclusion
Porcine small intestinal submucosa (SIS) grafting is a highly effective and biologically elegant solution for deep melting corneal ulcers in dogs and cats. It reliably halts stromal dissolution, seals perforations, and—most importantly—restores excellent corneal transparency while preserving vision in 100 % of cases. Compared with traditional conjunctival grafts, SIS offers superior optical outcomes with comparable safety, making it the preferred tectonic and regenerative biomaterial in modern veterinary corneal surgery.
