Sclera & Episclera in Dogs & Cats: The Eye’s Tough Outer Coat
Sclera & Episclera in Dogs & Cats
1.Sclera: Gross Structure and Composition
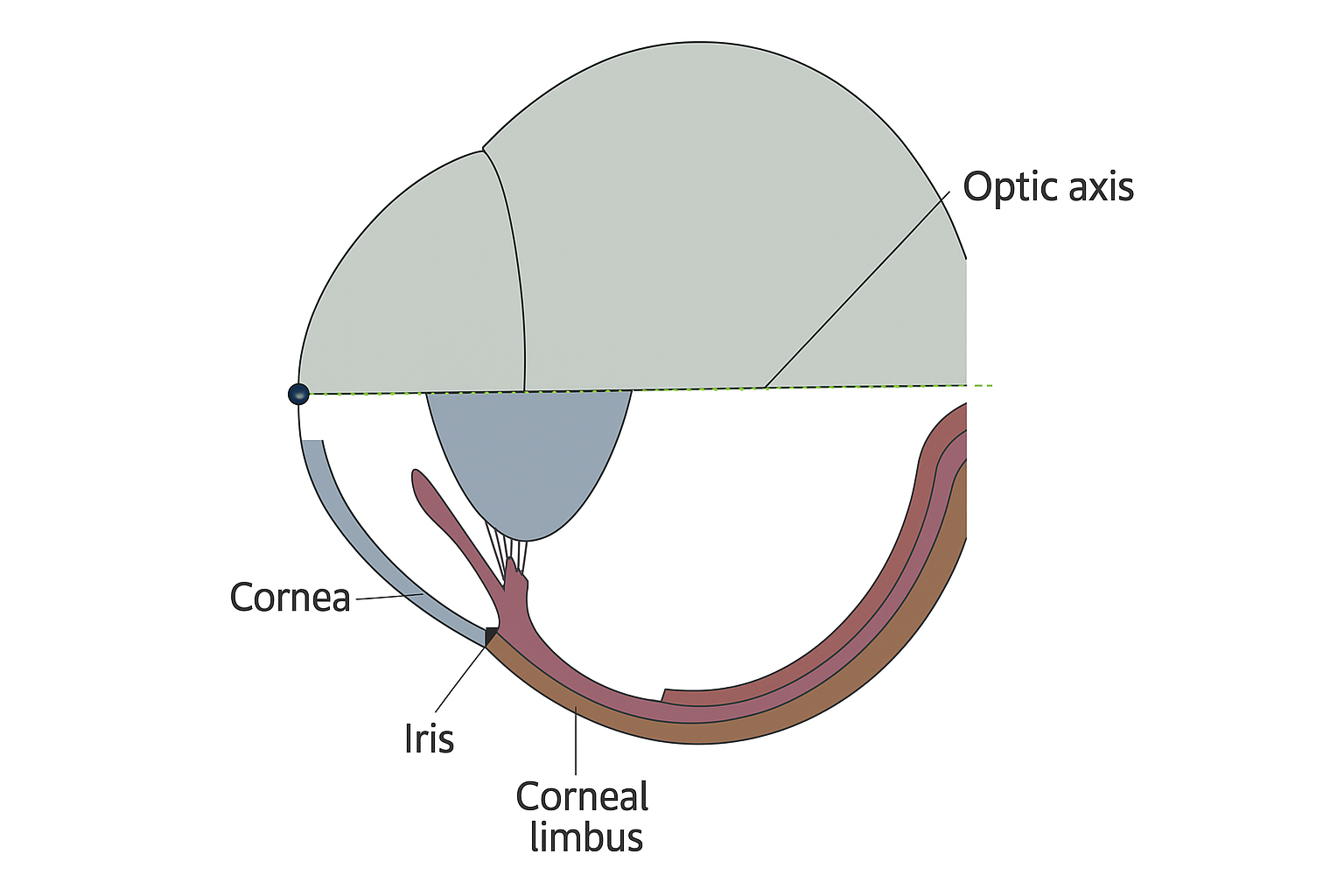
The sclera, which comprises nearly 85% of the globe’s external surface area in both dogs and cats, is a dense, irregularly arranged connective tissue constructed predominantly of type I collagen, interspersed with elastic fibers, proteoglycans, and scattered fibroblasts. In contrast to the highly regular collagen lattice of the cornea, scleral collagen fibers are woven in a multidirectional pattern, imparting both opacity and the viscoelasticity necessary for withstanding fluctuations in intraocular pressure and external trauma.
The thickness of the sclera varies regionally, measuring up to 0.8 mm at the posterior pole but thinning to approximately 0.3 mm near the equator and anterior to the rectus muscle insertions—a feature that creates physiologic “weak points” exploited by certain pathological processes such as staphyloma formation or retinal detachment.
Melanocytes, more prevalent in certain canine breeds and concentrated at the limbus, confer a slate-grey or bluish tint to the sclera, whereas cats typically exhibit less pigment except at the limbus or in melanotic conditions. Unlike the cornea, the sclera is avascular, relying on diffusion from the episcleral and choroidal vessels for metabolic exchange.
2.Episclera: Vascular Interface and Clinical Significance
Superficial to the sclera, the episclera constitutes a thin, highly vascular connective tissue sheath, replete with a plexus of arterioles and venules that communicate with the conjunctival and ciliary circulations. This vascularization is clinically significant, not only as a potential route for immune cell trafficking and drug absorption, but also as the site of origin for inflammatory or immune-mediated diseases such as episcleritis.
In addition, the episclera, by virtue of its loose collagen arrangement, provides a low-resistance plane for surgical manipulation (e.g., scleral buckling, subconjunctival injections) and is implicated in the pathogenesis and clinical appearance of “ciliary flush” and deep episcleral congestion—signs that are diagnostically important for distinguishing superficial from deep ocular pathology.
Integration with Adjacent Structures
The sclera is continuous anteriorly with the cornea at the limbus, where its irregular collagen transitions abruptly into the highly organized corneal stroma, and posteriorly with the dura of the optic nerve sheath. It serves as the insertion site for the extraocular muscle tendons, provides attachment for the ciliary body via the scleral spur, and supports the choroid and retina internally. Tenon’s capsule, a fascial envelope external to the episclera, facilitates frictionless globe rotation within the orbit, a feature especially critical for maintaining precise ocular motility.
Cellular and Biochemical Features
The scleral stroma, though sparsely cellular, is maintained by a population of fibroblasts responsible for the synthesis, remodeling, and repair of extracellular matrix components. Melanocytes—though less numerous than in the uvea—can accumulate with age, disease, or chronic inflammation, sometimes confounding clinical differentiation from intraocular or orbital melanosis.
Proteoglycans, including decorin and biglycan, modulate the hydration, spacing, and tensile strength of the collagen matrix; their dysregulation—whether from metabolic disease, systemic collagen disorders, or iatrogenic injury—may contribute to altered biomechanical properties and increased susceptibility to ectasia or rupture.
Unlike the cornea, the sclera lacks a true Bowman’s or Descemet’s membrane, rendering it more permeable to large molecules and less able to resist progressive stretching in the face of sustained intraocular pressure elevation.
Physiology and Biomechanics
The biomechanical role of the sclera and episclera is to resist deformation under physiologic and pathologic pressure gradients, thus preserving the globe’s geometry and protecting the delicate intraocular contents.
In healthy eyes, the sclera’s viscoelasticity accommodates transient increases in intraocular pressure—such as those experienced during blinking, eye movement, or mild trauma—by dispersing mechanical loads and allowing the globe to temporarily “give” without incurring permanent damage.
Chronic elevation of intraocular pressure, as seen in glaucoma, leads to progressive thinning and expansion of the sclera, particularly at the lamina cribrosa, which in turn precipitates optic nerve cupping and visual field loss.
These biomechanical principles underpin the pathophysiology of a host of ophthalmic conditions and highlight the necessity of monitoring scleral thickness and integrity in chronic disease states.
Fluid and Drug Dynamics
Despite its relative avascularity, the sclera—by virtue of its hydration and the vascularity of the overlying episclera—permits the slow, passive diffusion of fluids, drugs, and even immune cells.
This property has been leveraged in the development of transscleral and subconjunctival drug delivery systems, which are now increasingly employed for both anti-inflammatory and anti-glaucoma therapeutics in small-animal practice.
However, the same permeability renders the sclera susceptible to infiltration by infectious agents or neoplastic cells, emphasizing the dual-edged nature of this physiological feature.
Pathophysiological Perturbations
Episcleritis and Scleritis
- Episcleritis and scleritis, although uncommon in dogs and rare in cats, are important inflammatory conditions that may present acutely or insidiously.
- Episcleritis—most often idiopathic and believed to be immune-mediated (with a predilection for certain breeds, such as Collies)—is characterized clinically by sectoral or diffuse episcleral thickening, congestion, and minimal discomfort.
- Scleritis, which may be infectious (bacterial, fungal), immune-mediated, or secondary to adjacent neoplasia, typically presents as painful, diffuse scleral swelling that may extend to involve the cornea, uvea, or even the retina.
- Failure to promptly recognize and treat these conditions risks irreversible vision loss, globe perforation, or extension to adjacent orbital structures.
Scleral Ectasia and Staphyloma
Chronic glaucoma or inherited collagenopathies predispose the sclera to focal thinning (ectasia) and bulging (staphyloma), particularly at anatomic “weak points.”
Such structural compromise increases the risk for retinal detachment and complicates both medical and surgical management of the underlying disease.
Neoplasia and Degenerative Disorders
Primary scleral neoplasms—including melanomas and fibrosarcomas—are rare, whereas secondary extension from intraocular or orbital tumors is more commonly observed.
Dystrophic mineralization or calcification of the sclera, while infrequent, is occasionally seen in geriatric or systemically ill animals, and may pose diagnostic challenges.
Diagnostic Paradigm
A systematic diagnostic approach to scleral and episcleral disease begins with careful, well-illuminated inspection and palpation, followed by the application of topical phenylephrine to distinguish conjunctival from episcleral vascular congestion.
Ultrasound biomicroscopy and ocular ultrasonography provide non-invasive assessment of scleral thickness, the presence of staphylomas, or mass lesions.
Histopathologic examination, following biopsy or fine-needle aspiration, remains the gold standard for diagnosing neoplastic or infiltrative processes, while cytologic evaluation may be informative in cases of infectious or granulomatous scleritis.
References
Maggs DJ, Miller PE, Ofri R. Slatter’s Fundamentals of Veterinary Ophthalmology. 4th ed. Elsevier; 2008.
Gelatt KN, Gilger BC, Kern TJ, editors. Veterinary Ophthalmology. 6th ed. Wiley-Blackwell; 2021.
